My 2025 Functional Blood Work: A High-Performer’s Guide to Liver and Gallbladder Heal - Part 4
In Part 1, I unpacked the signs of an overactive immune system.
In Part 2, I explored my kidney markers and why “dysfunction” might be misleading.
In Part 3, I looked at my GI function (gut health) and my sub-optimal total protein.
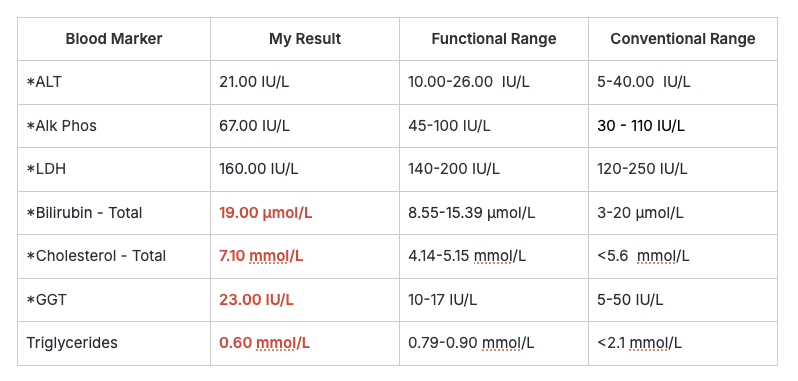
This week, we’re reviewing my liver and gallbladder results. According to my Functional Blood Analysis Report, my liver function has a 56% probability of dysfunction and my gallbladder has a 50% probability of dysfunction.
Not catastrophic. But not optimal either. And when you're training hard, running a business, parenting, and pushing for growth, suboptimal can catch up to you.
Liver Function Markers
Here are the markers used in the algorithm that looks at liver function.
Gallbladder Function Markers
Here are the markers used in the algorithm that looks at gallbladder function.
I've already covered some of these markers in part 1, part 2 and part 3.
Albumin (Low)
What It Is: Albumin is a protein made by the liver that helps with fluid balance, nutrient transport, and antioxidant defense.
Why It Matters: Low albumin can be an early marker of liver stress, chronic inflammation, or impaired nutrient absorption. It often drops before conventional liver enzymes show anything wrong.
Why Mine Might Be Low
Chronic immune load (gut stress, EBV recovery, histamine issues)
Liver pressure from detox demands, creatine byproducts, and a high-protein diet
Gut absorption issues (covered in Part 3)
What I’m Doing About It
Supporting detox: NAC, B-complex, sauna
Supporting digestion: HCl, enzymes, zinc
Reducing immune burden via gut protocol and stress management
Tracking trends over time, not just one result
Bottom Line: My low albumin reflects a high systemic load, not a lack of protein intake.
Bilirubin (High)
What It Is: Bilirubin is a yellow waste product from red blood cell breakdown. The liver processes it for excretion via bile.
Why It Matters: High bilirubin can indicate:
Sluggish liver detox pathways
Poor bile flow
Excess red blood cell turnover
Gallbladder Connection
Thick, stagnant bile increases risk of gallstones (especially pigment stones)
Poor bile flow = gallbladder congestion
Detox bottlenecks worsen histamine intolerance and toxin sensitivity
What I’m Doing:
Supporting phase 2 detox: NAC, B-complex, hydration, sauna
Enhancing bile flow: HCl, enzymes, bitters
Minimising liver stress: avoiding alcohol, excess sugar, and meds
Bottom Line: Likely a functional congestion, not a disease. My liver is working hard but needs better rhythm and support.
Cholesterol - Total (High)
What It Is: Cholesterol is essential for hormone production, vitamin D synthesis, brain health, and cell function. The liver makes 75% of your cholesterol and converts it into bile acids.
Why It Matters: High cholesterol can:
Thicken bile (when bile salts are low)
Increase gallstone risk (cholesterol stones)
Impair bile flow and fat-soluble vitamin absorption
Why Mine Might Be High:
High-protein, animal-based diet (red meat, eggs, liver)
Hormone repair and tissue recovery post-EBV
Natural genetic variance
Gallbladder Connection
Sluggish, thick bile stresses the gallbladder
May cause bloating, pale stools, or fatigue after fatty meals
Bottom Line: This isn’t about cardiovascular risk. It’s about bile function and liver load.
Gamma-Glutamyl Transferase (GGT) (Slightly High)
What It Is: GGT is a sensitive early marker for liver strain, oxidative stress, and bile stasis. It often elevates before ALT/AST.
Why It Matters
Indicates possible toxin or supplement load
May signal early gallbladder congestion
Correlates with oxidative stress around liver and bile ducts
Gallbladder Connection
High GGT = sluggish bile = more gallbladder strain
May explain symptoms like brain fog or nausea after fatty meals
What I’m Doing
Taking NAC, vitamin C, alpha-lipoic acid
Using sauna for gentle detox
Supporting bile with bitters and magnesium
Avoiding alcohol and unnecessary supplements
Bottom Line: Slightly elevated GGT is a nudge to respect the load I’m placing on my liver.
Triglycerides (Low)
What It Is: Triglycerides are fats in the blood, used for energy. Bile release is triggered by fat, so low triglycerides = less bile stimulation.
Why It Matters
Weak bile signals = sluggish gallbladder
May contribute to poor fat digestion and gallbladder congestion
Why Mine Might Be Low
Low-carb, high-protein diet
High fat metabolism from training
Possibly low fat intake or absorption
What I’m Doing
Increasing healthy fats: egg yolks, fatty fish, olive oil, liver
Supporting bile flow with choline, taurine, bitters
Ensuring consistent fat intake across meals
Bottom Line: Low triglycerides aren't bad, but combined with other markers, they hint at gallbladder under-stimulation.
Ferritin (High)
What It Is: Ferritin stores iron, mostly in the liver. High levels can signal inflammation, iron overload, or liver strain.
Why It Matters:
Excess iron gets stored in organs, especially the liver
Can contribute to fibrosis, cirrhosis, and liver dysfunction
What I’m Doing
Blood donations (I carry the hemochromatosis gene)
Supporting detox: NAC, milk thistle, curcumin, glutathione
Rotating protein sources
Monitoring markers every 6–12 months
Bottom Line: Managing iron stores is key for my long-term liver health.
Total Protein (Low)
What It Is: Measures albumin and globulins — proteins made by the liver and immune system.
Why It Matters
Can reflect liver underfunction, poor gut absorption, or immune stress
What I’m Doing
Supporting liver and gut (as above)
Tracking over time
Bottom Line: Another clue pointing to the liver-gut-immune load I'm carrying.
Final Reflection: Rhythm, Not Just Recovery
My liver and gallbladder aren’t failing. They’re just overworked.
Training, parenting, building a business, I’m often in output mode. But the liver doesn’t thrive in overdrive.
It needs:
Consistent meals
Strategic fasting windows
Parasympathetic support (sauna, breathwork, evening wind-down)
This isn’t about perfection. It’s about rhythm.
I'm learning to live in a way that supports my biology, not just my ambitions. And that’s a lesson worth sharing. In the next post I’ll be taking a look at my sex hormones and adrenals.